Trochanteric Fracture Causes, Symptoms & Treatment Options
A greater trochanteric fracture is an injury to the bony prominence on the upper femur where the hip abductor muscles attach, often caused by a direct fall onto the side of the hip. Common in older adults, it leads to pain and mobility issues. Accurate imaging and timely management aid recovery and function.
Start with our quick Symptom Assessment or connect directly with an Upswing Coach today.
Request an AppointmentReady to take the next step?
Start your symptom assessment or connect with a coach instantly.
Find Relief TodayOverview
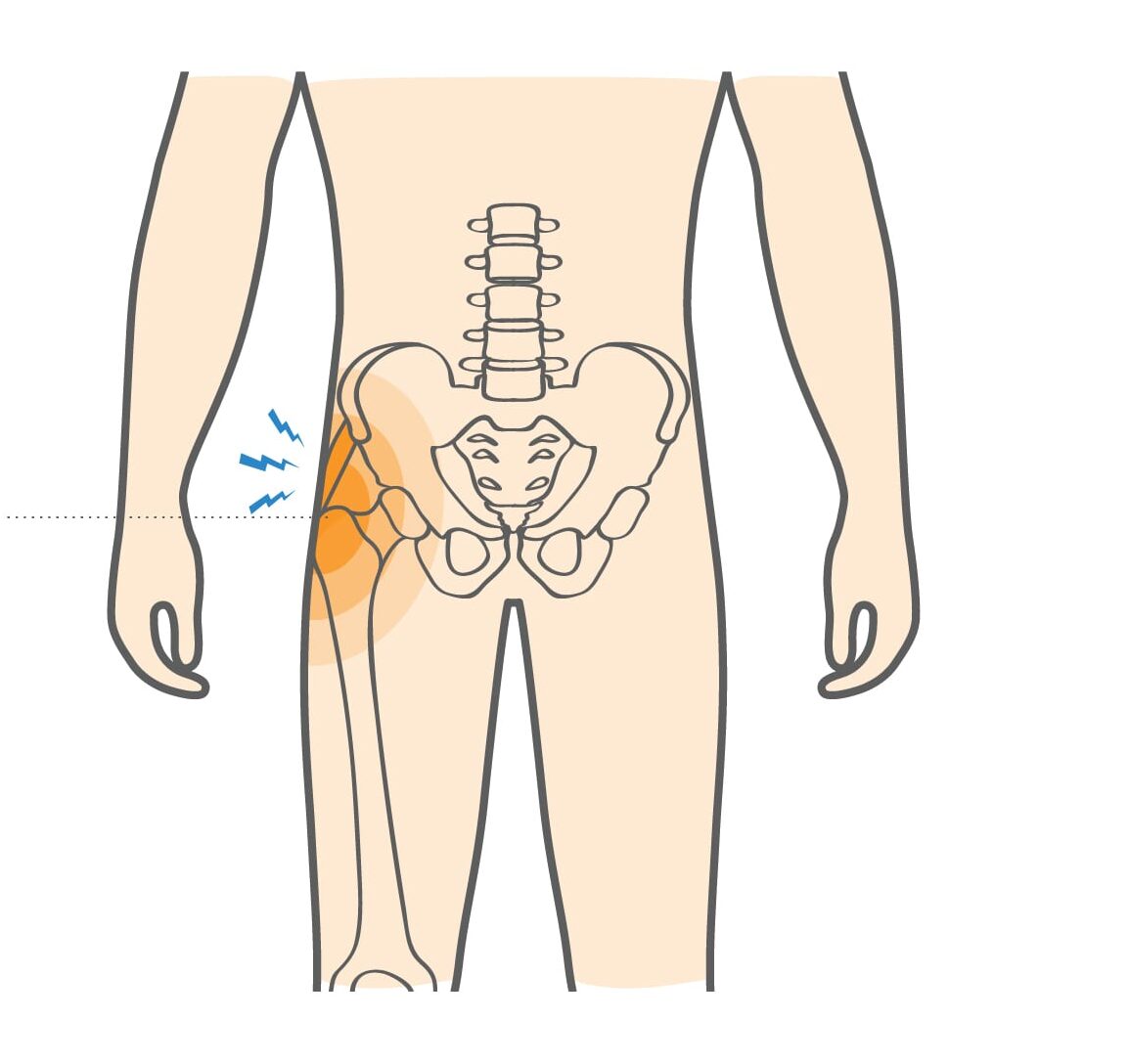
The greater trochanter is a prominent bony projection located on the lateral aspect of the proximal femur , forming an essential part of the hip structure and easily palpable on the outer surface of the thigh. It is a primary attachment site for the gluteal tendons, contributing to hip stability and movement.
Pain in this region is often attributed to trochanteric bursitis or gluteal tendinitis, conditions commonly resulting from chronic overuse, repetitive microtrauma, or localized inflammation. In more severe cases, involving direct trauma, it may lead to a fracture of the greater trochanter, requiring clinical evaluation and appropriate orthopedic management.
What causes Trochanteric Fracture?
Isolated greater trochanter fractures are uncommon and may occur alone or as part of a more extensive hip injury. They usually result from high-energy trauma, such as a fall from a height, a direct blow to the side of the hip, or a motor vehicle accident. While often seen in older adults with fragile bones, younger individuals may also experience this fracture following a significant impact.
- How the Injury Occurs: The fracture typically develops when a strong external force is transmitted to the lateral hip, disrupting the bone and surrounding tissues. Sometimes, a sudden and forceful muscle contraction during a fall can also contribute to the injury.
- Common Everyday Causes: These injuries may result from daily activities such as slipping in the shower, missing a step, or falling from household furniture. Workplace incidents, including ladder or scaffold falls, are also frequent causes.
- Sports Commonly Associated: High-impact sports like skiing, football, or contact-based disciplines can lead to similar injuries due to sudden collisions or awkward landings on the hip.
Symptoms
Patients with a fracture of the greater trochanter typically experience sharp, localized pain on the outer aspect of the hip, often accompanied by marked tenderness upon touch. Weight-bearing becomes painful, though partial mobility may still be possible. If discomfort radiates into the groin, it may indicate a more extensive hip fracture involving deeper structures.
Common symptoms of a greater trochanteric hip fracture include:
- Painful limp while bearing weight – Patients often walk with a noticeable limp due to pain and weakness in the hip muscles.
- Bruising or swelling over the lateral hip – The affected area may appear discolored or swollen due to soft tissue injury and internal bleeding.
When to see a doctor
If you experience a direct impact to the outer hip followed by immediate pain, swelling, and difficulty bearing weight, it may indicate a fracture of the greater trochanter or another hip injury. Medical evaluation should be sought promptly. During nights, weekends, or after-hours, visit an urgent care center if available, or proceed to the nearest emergency department.
Avoid walking or putting weight on the affected leg if it causes severe pain. If you have crutches and know how to use them safely, do so without bearing weight. Otherwise, seek assistance from a family member to reach medical care or contact emergency services for transportation.
A healthcare professional, such as a doctor, physician assistant, or nurse practitioner, will assess the injury, check for tenderness, and likely order an X-ray. If the X-ray appears normal but a fracture is still suspected, advanced imaging like a CT scan or MRI may be required for confirmation.
Non-operative treatment
When an isolated greater trochanter fracture is identified, the doctor will determine whether surgical repair is necessary. In cases where the fracture is nondisplaced, visible on the X-ray as a fine line without bone separation, conservative management is often appropriate. The physician may recommend a short observation period with repeat imaging after a few days to confirm that the fracture remains stable.
During this time, limited weight-bearing with crutches or a walker is advised to prevent displacement. Rest, ice application, and prescribed pain medication can help manage discomfort and swelling. A follow-up appointment is typically scheduled within 7 to 10 days to re-evaluate healing through X-ray imaging.
Surgical intervention may be required if the follow-up scan shows any displacement or progression. As healing progresses, a structured physical therapy program may be introduced to restore hip strength, flexibility, and normal gait function.
Surgical Treatment
Surgical repair is usually indicated if initial or follow-up X-rays reveal a fracture of the greater trochanter with clear bone separation or displacement. Surgery aims to restore bone alignment, ensure stability, and promote healing.
Typically, ORIF is achieved using two or three lag screws or similar orthopedic implants to secure the fragments in place. This stabilization allows early healing, which generally occurs within 6 to 8 weeks under proper postoperative care.
In some cases, especially with complex or unstable fractures, additional fixation devices such as plates or cables may be used based on the surgeon’s assessment.
Recovery
With appropriate treatment, whether managed conservatively or surgically, greater trochanter fractures heal well without significant complications. Healing progress is monitored through periodic X-rays to confirm bone union.
Once the fracture is stable, your doctor will likely recommend a structured physical therapy program to restore flexibility, strength, and normal hip function. As pain subsides and strength improves, a gradual return to daily activities and low-impact exercises is encouraged.
Most patients fully recover within 4 to 6 months, although complete restoration of muscle strength and balance may take slightly longer, depending on age, bone health, and adherence to rehabilitation guidelines.
Dr. Jay Kimmel is a board-certified orthopedic surgeon specializing in sports medicine, arthroscopic surgery, and shoulder and knee disorders. He completed his orthopedic training at New York-Presbyterian/Columbia University Medical Center and a Sports Medicine Fellowship at Temple University.
Dr. Kimmel previously served as the Director of the Connecticut Sports Medicine Institute at Saint Francis Hospital and has held faculty appointments as Clinical Assistant Professor in the Departments of Orthopedics and Family Medicine at the University of Connecticut. He has extensive experience caring for athletes as a team physician for high school and collegiate programs and continues to teach in the athletic training departments at Westfield State University and Springfield College.
Find the Support You Need — Right When You Need It
Whether you’re managing pain for the first time, need ongoing guidance, or require expert medical care, we’re here to help you every step of the way.
ORTHO DIRECT
Video visit with an orthopedic doctor for advice and a care plan.
$30
/MonthMRI DIRECT
Fast, affordable MRI with orthopedic review. No insurance required.
$499
/MonthFrequently Asked Questions
How long does it usually take to walk again?
Patients usually begin light-weight bearing within a few weeks, progressing to normal walking over 6 to 12 weeks, depending on healing progress and physical therapy.
Will physical therapy help after treatment?
Absolutely. Physical therapy is key in restoring hip strength, flexibility, and balance, helping patients regain mobility faster and prevent stiffness.
Is surgery always required for this type of fracture?
Not always. Many isolated, non-displaced fractures heal successfully with rest, limited weight-bearing, and close follow-up under a doctor’s supervision.
Can I return to regular activities after recovery?
Yes, most patients return to their regular routines, including low-impact exercises, within a few months once bone healing and muscle strength are fully restored.