Shoulder dislocations occur when the head of the humerus (the long bone of the upper arm) completely leaves the glenoid cavity of the scapula (shoulder blade). Although the structure of the shoulder allows you greater range of motion for athletic activities, it is also at a higher risk of dislocations. A traumatic dislocation occurs when the head of the humerus is forcefully pushed out of its socket due to an impact, such as a tackle in football, or a traumatic injury, like a fall.
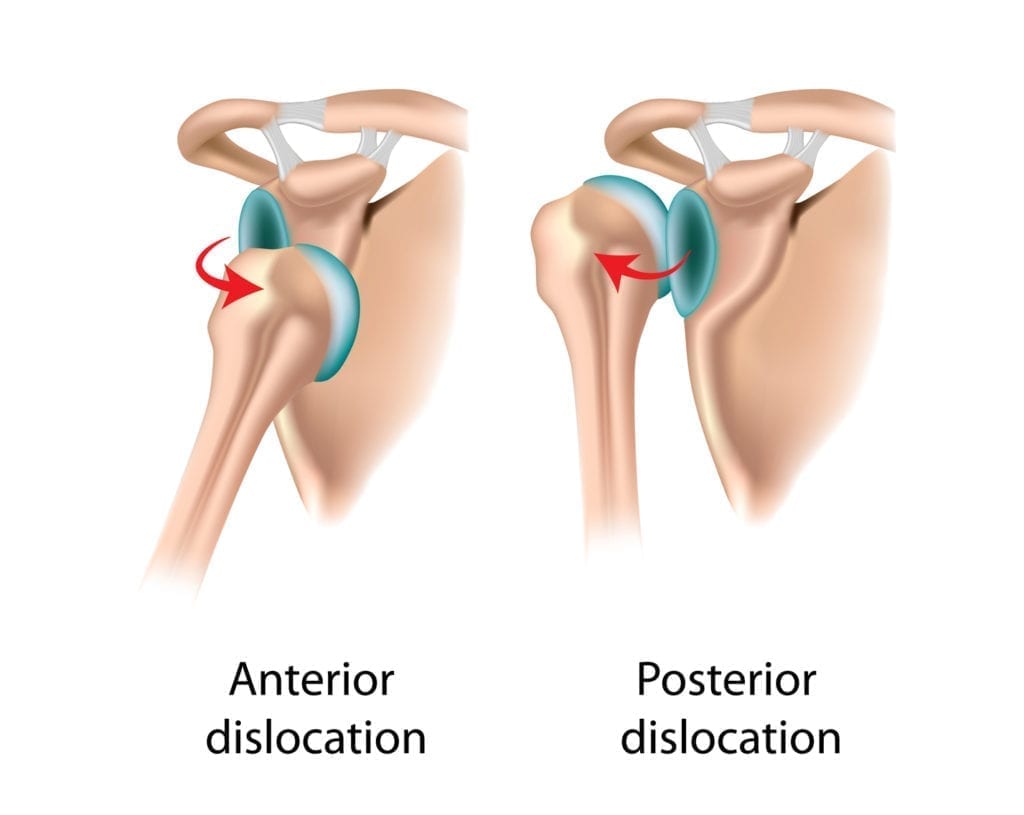
The shoulder can become dislocated in one of two directions:
- Anteriorly (through the front of the joint)
- Posteriorly (through the back of the joint)
Anterior shoulder locations are much more common than posterior shoulder locations.