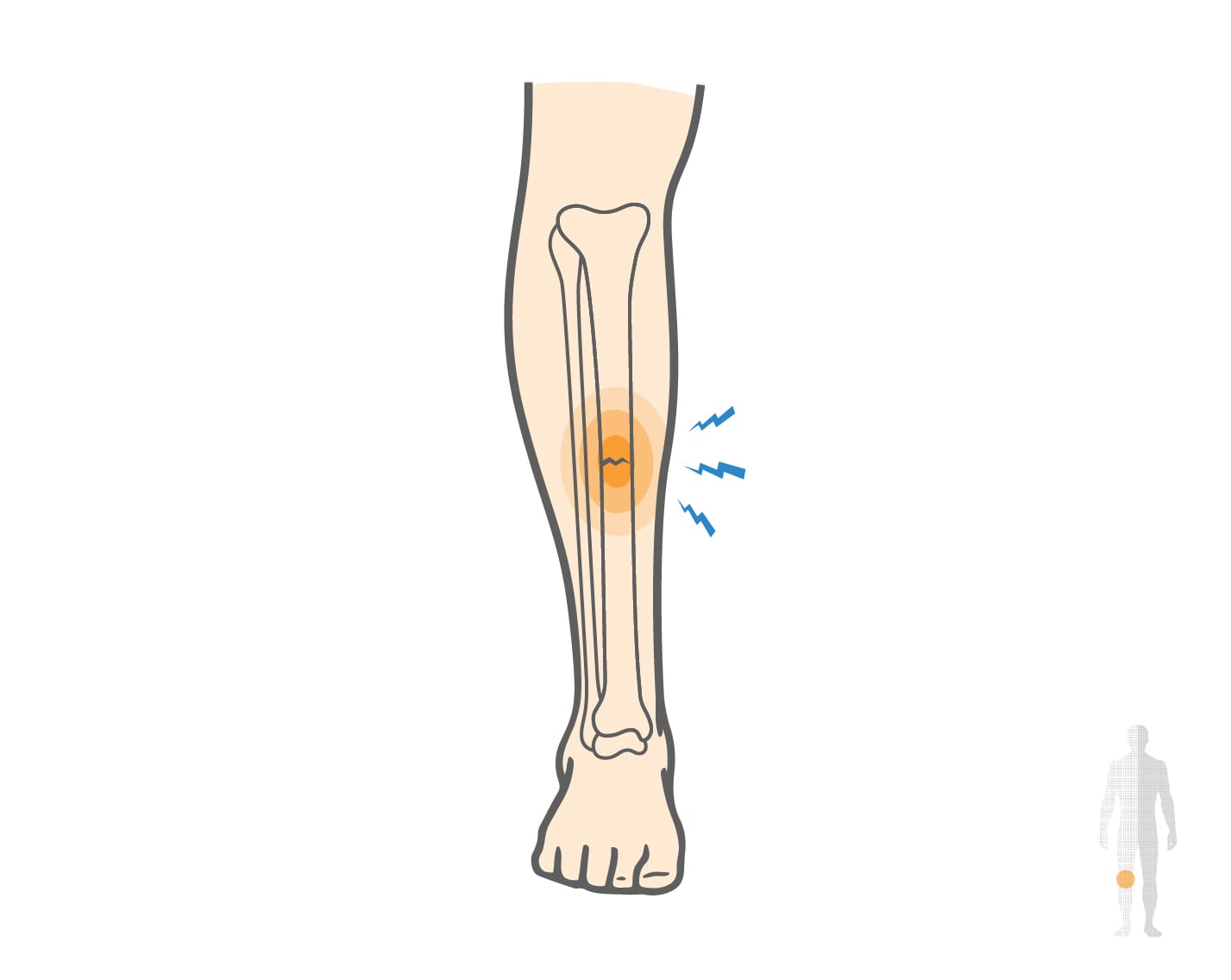
Stress Fracture of the Tibia Causes, Symptoms & Treatment
Tibial stress fracture is a common overuse injury, frequently observed in athletes involved in repetitive impact activities such as running or jumping. It results from cumulative mechanical stress exceeding bone remodeling capacity. Early clinical evaluation and imaging diagnosis are essential to prevent progression and ensure optimal recovery.
Start with our quick Symptom Assessment or connect directly with an Upswing Coach today.
Request an AppointmentReady to take the next step?
Start your symptom assessment or connect with a coach instantly.
Find Relief TodayOverview
A stress fracture, represents a partial cortical break resulting from repetitive mechanical loading that exceeds the bone’s capacity for repair. The tibia, the primary weight-bearing bone of the lower leg, is particularly susceptible. This condition is commonly observed in athletes engaged in high-impact or endurance activities.
Repetitive stress without adequate rest & load management leads to microdamage accumulation, resulting in pain, swelling, and functional limitation. Early recognition and appropriate management are essential to prevent a complete fracture and ensure a safe return to physical activity.
What causes Stress Fracture of the Tibia?
A shin stress fracture of the tibia generally occurs when repetitive loading exceeds the bone’s natural ability to remodel and recover. Prolonged high-impact activities or sudden increases in training intensity can create microtrauma in the bone cortex.
Athletes are particularly vulnerable during training volume or surface type transitions. Factors such as reduced bone mineral density, nutritional deficiencies, or improper footwear can increase the risk of injury.
- How the Injury Occurs: The repetitive mechanical stress on the tibia during weight-bearing activity leads to an imbalance between bone resorption and formation. Over time, microcracks accumulate within the bone structure, ultimately progressing to a stress fracture if not adequately managed.
- Common Everyday Causes: Stress fractures of the tibia can also occur in military recruits during basic training, dancers performing repetitive jumps, or individuals whose occupations involve prolonged standing or marching on hard surfaces.
High-Risk Sports and Activities
Stress fractures of the tibia are most frequently associated with the following sports:
- Short-distance running/sprinting: Rapid acceleration and deceleration produce concentrated forces on the tibial shaft.
- Cross-country running: Continuous long-distance impact on uneven terrain leads to repetitive stress.
- Basketball: Frequent jumping and abrupt directional changes subject the tibia to high compressive loads.
- Soccer: Repetitive kicking, sprinting, and tackling generate cumulative microtrauma on the lower leg.
Symptoms
Pain is the primary symptom of a tibial stress fracture, often developing gradually and concentrating in a specific area of the shin. Initially, discomfort may only appear toward the end of physical activity, but over time, it can begin earlier and persist longer. Other commonly observed symptoms include:
- Pain that worsens with activity: Discomfort intensifies during running, jumping, or prolonged weight-bearing.
- Progressive pain: Both the severity and duration of pain increase as the fracture develops.
- Localized swelling: Mild to moderate swelling may occur directly over the affected site, indicating inflammation.
When to see a doctor
If you experience persistent pain in a specific area of your shin that gradually worsens, it is important to seek medical evaluation. During the examination, the physician will assess the affected area, ask about the onset of leg pain and the activity-related nature of the pain, and perform a physical assessment to pinpoint the fracture site.
While an X-ray may be requested, small stress fractures may not be visible initially. Additional imaging, such as a bone scan or magnetic resonance imaging (MRI), may be necessary to confirm the diagnosis.
Non-operative treatment
Treatment for a stress fracture of the tibia focuses on pain relief and allowing the tibia to heal. This can usually be accomplished through non-surgical treatments. Conservative treatments include:
- Rest from activities and sports that place stress on the lower leg.
- Wearing a walker boot, with or without crutches, until pain resolves
- Applying ice for 15 minutes two or three times daily, especially after any activity
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can help relieve pain and inflammation
- Increasing calcium in your diet (e.g., from foods like broccoli, yogurt, cheese, and dairy)
Try these exercises to help address your condition:
Below is a PDF of the Exercise Program
Surgical Treatment
Surgical intervention is rarely required for stress fractures of the tibia, as most cases respond well to conservative management. Surgery may only be considered in exceptional situations, such as when the fracture fails to heal with rest and rehabilitation, or in cases of severe fracture displacement or complications.
Recovery
The cornerstone of recovery is rest from activities that place stress on the tibia, allowing the bone sufficient time to heal. For runners, this often means refraining from running for four to six weeks, sometimes several months. A gradual return to activity, guided by a physician or physical therapist, is essential.
This may include progressively increasing exercise intensity, limiting frequency, and performing activities on softer surfaces. Substituting low-impact exercises, such as swimming or cycling, can help maintain fitness while reducing stress on the tibia.
Strengthening exercises targeting the muscles and tendons surrounding the tibia are also important to support bone health and prevent future injury. Athletes remain at higher risk for recurrent stress fractures, so proper warm-up and cool-down routines, along with a nutrient-rich diet high in calcium, are critical components of long-term prevention.
Dr. Jay Kimmel is a board-certified orthopedic surgeon specializing in sports medicine, arthroscopic surgery, and shoulder and knee disorders. He completed his orthopedic training at New York-Presbyterian/Columbia University Medical Center and a Sports Medicine Fellowship at Temple University.
Dr. Kimmel previously served as the Director of the Connecticut Sports Medicine Institute at Saint Francis Hospital and has held faculty appointments as Clinical Assistant Professor in the Departments of Orthopedics and Family Medicine at the University of Connecticut. He has extensive experience caring for athletes as a team physician for high school and collegiate programs and continues to teach in the athletic training departments at Westfield State University and Springfield College.
Find the Support You Need — Right When You Need It
Whether you’re managing pain for the first time, need ongoing guidance, or require expert medical care, we’re here to help you every step of the way.
ORTHO DIRECT
Video visit with an orthopedic doctor for advice and a care plan.
$30
/MonthMRI DIRECT
Fast, affordable MRI with orthopedic review. No insurance required.
$499
/MonthFrequently Asked Questions
What are the common symptoms of a tibial stress fracture?
Typical symptoms include localized pain along the shin, swelling, tenderness to touch, and discomfort that worsens with physical activity and improves with rest.
Who is most at risk for developing a tibial stress fracture?
Athletes are at higher risk, especially runners or individuals who rapidly increase their training intensity or volume. People with low bone density or poor nutrition are also more susceptible.
How is a stress fracture of the tibia diagnosed?
A doctor may confirm the presence of a stress fracture by combining physical examination, patient history, and imaging tests like X-rays or MRI.
What is the typical treatment for a tibial stress fracture?
Treatment usually includes rest, avoiding high-impact activities, nutritional support, and sometimes physical therapy. In more severe cases, immobilization or further intervention may be needed.