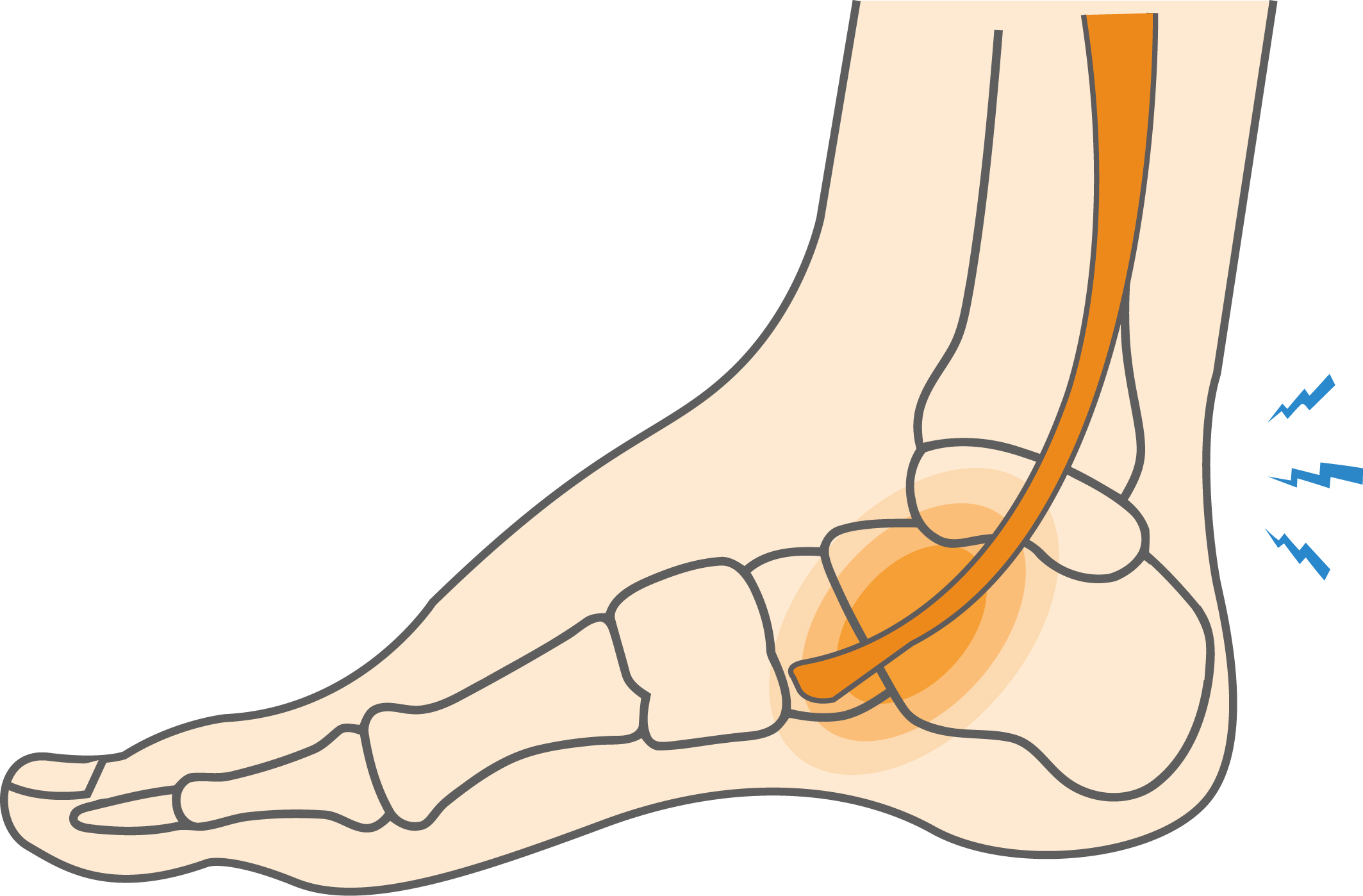
Tendons are strong, cord-like tissues that connect muscles to bones. The posterior tibial tendon runs from the calf muscles, down the inside of the ankle, and to the foot bones. This important tendon holds up your foot, maintains your arch, and is essential for walking. Dysfunction of the posterior tibial tendon is a common problem that happens when the tendon becomes inflamed or torn. It often leads to foot arch collapse or a flatfoot condition as the disease progresses. It often leads to foot arch collapse or a flatfoot condition as the disease progresses.Collapse of the arch of the foot occurs with increasing severity of tendonitis or rupture of this tendon. Doctors often classify a patient’s level of posterior tibial tendon dysfunction in four progressive stages of severity, with stage 4 representing the highest level of posterior tibial tendon failure.
Posterior Tibial Tendonitis Causes, Symptoms & Treatment
Tendons are strong, cord-like tissues that connect muscles to bones. The posterior tibial tendon runs from the calf muscles, down the inside of the ankle, and to the foot bones. This important tendon holds up your foot, maintains your arch, and is essential for walking. Dysfunction of the posterior tibial tendon is a common problem that happens when the tendon becomes inflamed or torn. It often leads to foot arch collapse or a flatfoot condition as the disease progresses. It often leads to foot arch collapse or a flatfoot condition as the disease progresses.
Overview
Overview
What causes Posterior Tibial Tendonitis?
Posterior tibial tendonitis is often triggered by tendon strain due to overuse. Dancers and athletes who play high-impact sports are at risk due to the stress on this tendon. An acute injury, such as a fall or collision, can also tear the posterior tibial tendon.
Posterior tibial tendon dysfunction is most common in these sports:
• Dancing
• Tennis
• Basketball
• Soccer
Symptoms
One of the hallmark symptoms is inner ankle pain, typically felt where the tendon runs along the inside of the ankle and foot. Additional signs include:
• Swelling
• Difficulty running or walking
• A gradual flattening of the arch
• In advanced cases, the heel may push outwards and pain may be felt on the outside of the foot

When to see a doctor
If left untreated, posterior tibial tendon dysfunction may worsen, and treatment will become more invasive. It’s essential to seek medical care early, especially if you experience persistent inner ankle pain or changes in foot shape. To diagnose, your doctor will take a medical history and ask about your physical activity. A physical examination will be conducted, looking for tenderness along your tendons, swelling, stiffness, and signs of deformity to your foot and ankle.
To test the integrity of the tendon, your doctor may ask you to stand on your affected foot and rise on your toes (called the single-limb heel rise). Another common test involves looking at your heel from behind to see if the fourth and fifth toes are visible. If they are, you may have lost your arch, a sign of advanced-stage dysfunction and foot arch collapse. To help confirm the diagnosis and detect the presence of arthritis, x-rays and other imaging tests, such as a magnetic resonance imaging (MRI) test, may be ordered.
Non-operative treatment
Non-surgical treatments are usually successful in treating posterior tibial tendon dysfunction in its earlier stages. Treatment focuses on allowing your tendon to heal as well as relieving pain and other symptoms. Avoiding activities that cause pain and place repeated stress on your foot is important for allowing the healing process to take place. Common treatments also include:
• Physical therapy with suggestive posterior tibial tendonitis exercises
• Using crutches if walking is painful
• Wearing a cast or special boot to immobilize and support your foot or orthotic shoe inserts with arch support
• Anti-inflammatory medication for pain relief
• Physical therapy
• In rare cases a cortisone injection, a powerful anti-inflammatory pain reliever, may be recommended
Try these posterior tibial tendonitis exercises to help address your condition:
Below is a PDF of the Exercise Program
Surgical Treatment
If conservative treatments aren’t successful within six months, or in advanced stages of posterior tibial tendon dysfunction, surgery may be considered. The type of surgery will depend on the stage of dysfunction. In earlier stages, a surgical procedure called debridement, which involves cleaning away and removing inflamed or torn tissue, may be effective. Another surgical procedure replaces the damaged posterior tibial tendon with a healthy tendon transferred from the foot.
In more advanced cases where the arch has collapsed, your surgeon may recommend osteotomy, which involves cutting and shifting bones in the foot to reconstruct the arch. In the most severe cases, surgeons may fuse the joints in your foot together, using screws and plates, to realign the foot and address flatfoot condition and tendon strain.
Recovery
Recovery from posterior tibial tendon dysfunction will depend on the stage of the disease and the type of treatment. Athletes treated conservatively usually can get back to normal activities within a few weeks. Advanced cases treated surgically may require a recovery that lasts three months or more. While outcomes from surgery are generally positive, some athletes with severe tendon damage may not regain their full range of motion or be able to return to high impact sports. Your doctor will advise on the type of surgery needed, the risks of surgery, and how to maximize your ability to achieve a full recovery.