Posterior Tibial Tendonitis Causes, Symptoms & Treatment
Posterior tibial tendonitis is a common overuse injury that often affects athletes and individuals with flatfoot deformities. Repetitive strain causes inflammation and pain along the inner (medial) aspect of the ankle, leading to gradual loss of tendon strength and function. While most cases respond to conservative treatment, surgical intervention may be necessary in advanced stages to restore tendon integrity and proper foot alignment.
Start with our quick Symptom Assessment or connect directly with an Upswing Coach today.
Request an AppointmentReady to take the next step?
Start your symptom assessment or connect with a coach instantly.
Find Relief TodayOverview
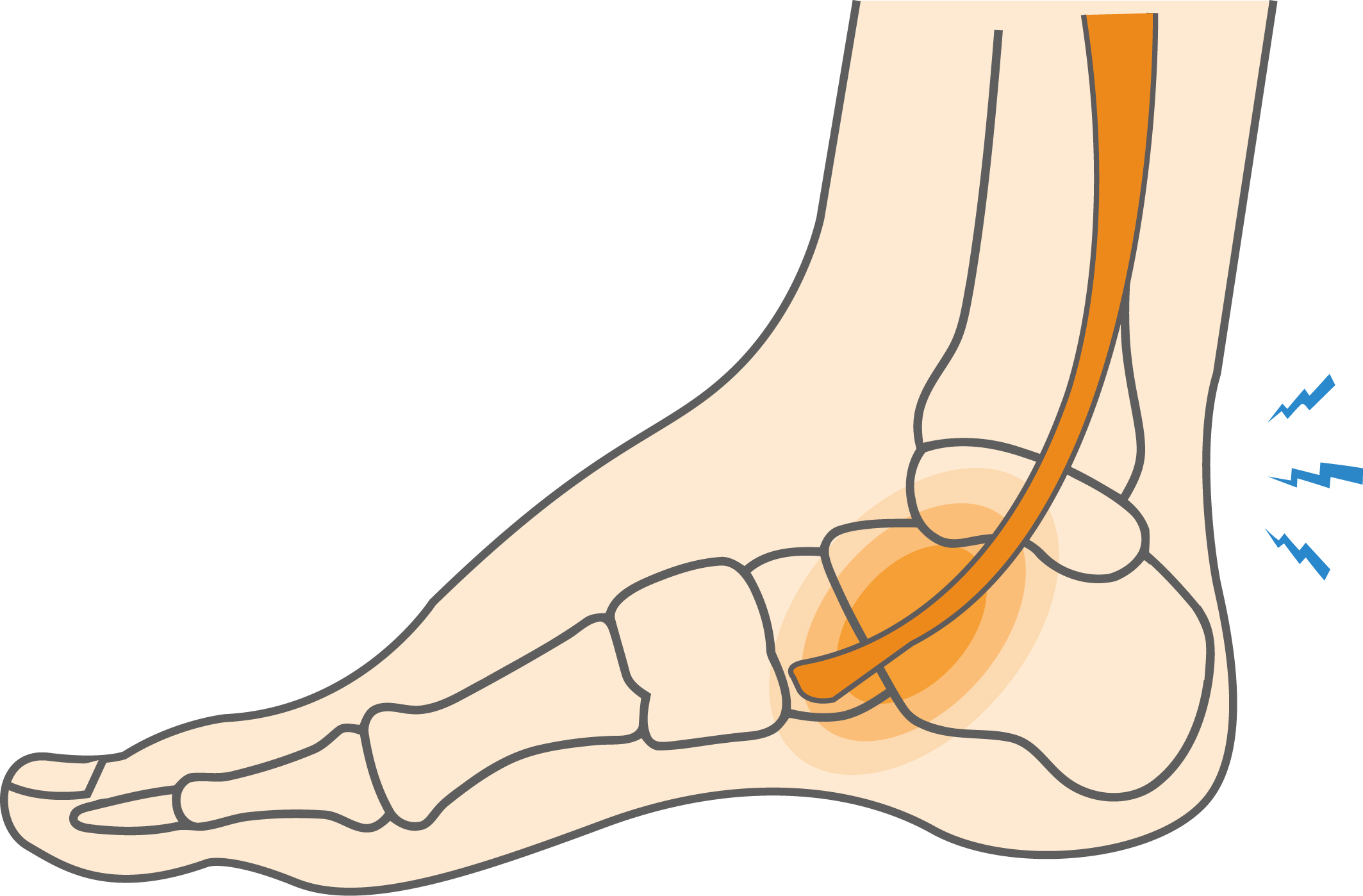
Tendons are strong, cord-like tissues that connect muscles to bones. The posterior tibial tendon runs from the calf, along the inside of the ankle, and attaches to the bones of the foot. It helps support the arch and is important for everyday walking.
When this tendon becomes inflamed or torn, the condition is known as posterior tibial tendon dysfunction. It often causes the arch to flatten, leading to a flatfoot deformity gradually. The arch collapses as the tendon becomes more damaged or completely ruptures.
Clinicians often classify posterior tibial tendon dysfunction (PTTD) into four progressive stages, with stage IV representing complete tendon failure.
What causes Posterior Tibial Tendonitis?
Posterior tibial tendonitis most often develops from repetitive strain or overuse of the tendon. Athletes and dancers involved in high-impact or repetitive foot movements are particularly at risk. In some cases, a single traumatic event, such as a fall or collision, can cause a partial or complete tear of the tendon.
- How the Injury Occurs: The condition results from repetitive stress, sudden trauma, or a combination of both. These forces lead to inflammation, tendon degeneration, and eventual weakening of the tendon’s ability to support the foot arch.
- Common Everyday Causes: Posterior tibial tendonitis is not limited to athletes. It is also common among individuals with flatfoot, obesity, or occupations that involve prolonged standing or walking, all of which place continuous strain on the tendon.
Posterior tibial tendon dysfunction is most common in these activities:
- Dancing: Repetitive jumping and pointe work place excessive load on the tendon, leading to inflammation and small tears.
- Tennis: Quick lateral movements and abrupt stops create significant stress on the tendon.
- Basketball: High-impact landings and rapid directional changes challenge tendon stability and function.
- Soccer: Continuous running, cutting, and pivoting motions contribute to chronic overuse and tendon irritation.
Symptoms
The main symptom of posterior tibial tendon dysfunction (PTTD) is pain along the inside (medial) aspect of the ankle, following the path of the tendon from the calf to the foot. As the condition progresses, additional signs and functional limitations may appear.
- Swelling: Localized inflammation and tenderness along the tendon, often accompanied by warmth around the affected area.
- Difficulty walking or running: Reduced tendon strength and stability make walking, running, or standing painful for long periods.
- Gradual flattening of the arch: The medial arch of the foot lowers over time as the tendon weakens.
- Advanced cases: The heel may shift outward (hindfoot valgus), and pain may develop along the outer side of the foot due to altered alignment and compensatory loading.

When to see a doctor
If left untreated, posterior tibial tendon dysfunction (PTTD) can progressively worsen, often leading to more complex or invasive treatment needs. Early medical evaluation is essential, especially when medial ankle pain persists or visible changes in foot alignment are noticed.
Diagnosis typically begins with a detailed medical history and an assessment of physical activity patterns. A clinical examination focuses on tenderness along the tendon, swelling, stiffness, and any foot or ankle deformity.
To assess tendon integrity, clinicians often perform a single-limb heel rise test, in which the patient stands on the affected foot and attempts to rise onto the toes. The inability to do so may indicate significant tendon weakness. Another observation involves viewing the heel from behind, if the fourth and fifth toes are visible from this angle, it may suggest arch collapse and advanced-stage dysfunction.
Imaging studies, such as X-rays or magnetic resonance imaging (MRI), are commonly used to confirm the diagnosis and evaluate for associated arthritis or structural abnormalities.
Non-operative treatment
Non-surgical management is often effective in the early stages of posterior tibial tendon dysfunction. The main objectives are reducing pain, controlling inflammation, and supporting tendon healing. Limiting activities that cause discomfort or repetitive strain on the foot is essential for recovery.
Common conservative treatments include:
- Physical therapy: Focused exercises to strengthen the posterior tibial tendon, improve flexibility, and restore proper foot alignment.
- Use of crutches: Recommended when walking is painful to minimize stress on the affected tendon.
- Immobilization: A cast, walking boot, or orthotic inserts with arch support may stabilize the foot and allow the tendon to heal.
- Anti-inflammatory medication: Helps manage pain and decrease localized swelling.
- Cortisone injection: In select cases, corticosteroid injections may be administered to control severe inflammation, though they are used cautiously to avoid tendon weakening.
For guided rehabilitation, specific posterior tibial tendonitis exercises can help strengthen the tendon and restore normal function.
A detailed Exercise Program is available in the PDF linked below:
Posterior Tibial Tendonitis Exercise Program (PDF)
Surgical Treatment
Surgery is considered when conservative management fails after approximately six months or in advanced stages of posterior tibial tendon dysfunction. The specific procedure depends on the extent of tendon damage and structural deformity.
- Tendon debridement: Removing inflamed or degenerated tissue in the early stages may relieve symptoms and restore partial tendon function.
- Tendon transfer: When the posterior tibial tendon is severely damaged, a nearby healthy tendon may be transferred to assume its role and restore foot support.
- Osteotomy: For patients with significant arch collapse, surgical realignment through precise cutting and repositioning of the foot bones helps reconstruct the arch and correct deformity.
- Joint fusion (arthrodesis): In severe or end-stage cases, fusing affected joints with screws or plates stabilizes the foot, alleviates pain, and prevents further collapse.
Postoperative rehabilitation typically includes immobilization, gradual weight-bearing, and targeted physical therapy to restore mobility and strength.
Recovery
Recovery from posterior tibial tendon dysfunction depends on the stage of the condition and the treatment approach. Patients managed conservatively often return to normal activities within a few weeks.
In advanced cases requiring surgery, recovery may take three months or longer. While surgical outcomes are generally favorable, individuals with severe tendon damage may experience limited restoration of the full range of motion or a reduced ability to resume high-impact activities.
Your physician will provide guidance on the appropriate surgical procedure, associated risks, and strategies to optimize functional recovery and long-term foot health.
Dr. Jay Kimmel is a board-certified orthopedic surgeon specializing in sports medicine, arthroscopic surgery, and shoulder and knee disorders. He completed his orthopedic training at New York-Presbyterian/Columbia University Medical Center and a Sports Medicine Fellowship at Temple University.
Dr. Kimmel previously served as the Director of the Connecticut Sports Medicine Institute at Saint Francis Hospital and has held faculty appointments as Clinical Assistant Professor in the Departments of Orthopedics and Family Medicine at the University of Connecticut. He has extensive experience caring for athletes as a team physician for high school and collegiate programs and continues to teach in the athletic training departments at Westfield State University and Springfield College.
Find the Support You Need — Right When You Need It
Whether you’re managing pain for the first time, need ongoing guidance, or require expert medical care, we’re here to help you every step of the way.
ORTHO DIRECT
Video visit with an orthopedic doctor for advice and a care plan.
$30
/MonthMRI DIRECT
Fast, affordable MRI with orthopedic review. No insurance required.
$499
/MonthFrequently Asked Questions
Is it possible to return to sports after treatment?
Yes. Many athletes recover fully with proper rehabilitation, gradually resuming activities while maintaining tendon strength and foot stability.
How long does recovery usually take?
Recovery varies depending on severity and treatment type. Mild cases may improve within weeks, while surgical cases typically require several months. With adherence to their recovery plan, most patients achieve good functional outcomes.
Can lifestyle changes help prevent worsening?
Yes. Avoiding repetitive stress, wearing supportive footwear, and performing tendon-strengthening exercises can protect the tendon and reduce the risk of progression.
Are surgical outcomes generally positive?
Yes. When indicated, modern surgical techniques usually restore foot alignment and tendon function, allowing most patients to return to daily activities and sports with reduced pain.