Lumbar Disc Herniation/Sciatica Causes, Symptoms & Treatment
A Lumbar disc herniation occurs when a disc in the lower back becomes damaged and bulges out of place. This pressure can irritate nearby nerves, causing sharp lower back pain, leg pain, or sciatica. Common symptoms include pain with movement, numbness, and muscle weakness. Most cases improve with rest, medication, and physical therapy, though some may require further treatment if the pain persists.
Start with our quick Symptom Assessment or connect directly with an Upswing Coach today.
Request an AppointmentReady to take the next step?
Start your symptom assessment or connect with a coach instantly.
Find Relief TodayOverview
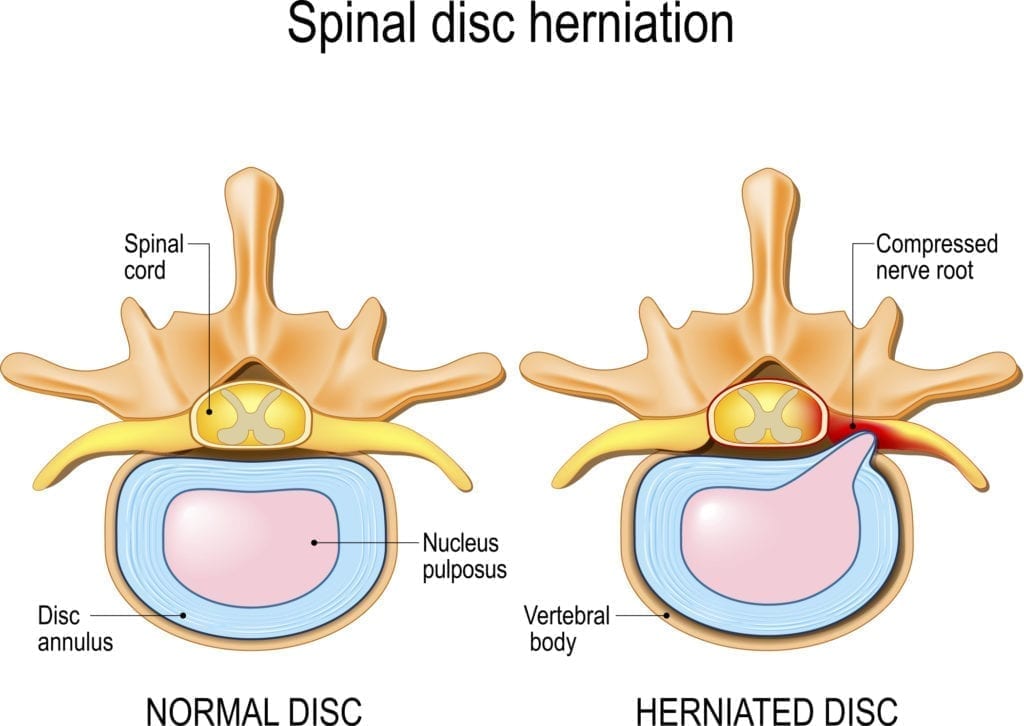
Back pain is one of the most common complaints among athletes and active individuals. A lumbar disc herniation, often called a slipped, ruptured, or herniated disc, is a frequent cause of this pain. The discs in your lower back sit between the vertebrae and act like cushions, allowing your spine to bend, twist, and absorb impact.
Each disc has a tough outer layer and a soft, jelly-like center. When the outer layer weakens or tears, the inner material can bulge out. This bulge may press on the spinal cord or nearby nerves, causing symptoms such as sharp lower back pain or pain that radiates down the legs. When leg pain occurs, it is often referred to as sciatica.
In many people, a lumbar herniated disc develops gradually due to aging or repeated stress, while in others, it may occur suddenly from a lifting injury or awkward twist.
What causes Lumbar Disc Herniation/Sciatica?
Lumbar Disc Herniation can develop gradually or suddenly. Although it can happen at any age, adults over 30 years of age are more at risk because the discs naturally weaken over time. Simple daily movements or heavy lifting can sometimes trigger a tear in an already stressed disc.
1. How the Injury Occurs
- Disc degeneration over time: As people age, discs lose water content and become less flexible, making them more likely to rupture.
- Improper lifting techniques: Bending or twisting the spine while lifting something heavy can create too much pressure on the lumbar discs.
- Sudden heavy strain: A sharp, forceful movement, like lifting a heavy object or twisting quickly, may cause a tear.
- Trauma or impact: Although less common, a fall, sports collision, or blow to the back can damage the disc.
2. Common Everyday Causes
- Frequent bending or twisting during household chores
- Sitting for long hours with poor posture
- Repetitive lifting at work
- Driving for long periods increases pressure on the lumbar spine
- Weak core muscles that fail to support the lower back
Sports That Commonly Lead to Lumbar Herniated Discs
These activities place repeated stress on the lower back, increasing the likelihood of disc injuries:
- Racket sports: Tennis, racquetball, and squash involve quick twisting motions.
- Hockey: Strong rotational movements and impact increase risk.
- Football & Rugby: Heavy contact and sudden directional changes strain the spine.
- Basketball: Jumping and landing compress the lower back.
- Baseball: Repeated twisting, especially while batting.
- Weightlifting: Heavy loads, especially deadlifts or squats, can overload the spine.
- Golf: Strong rotational swings stress the lumbar area.
Swimming: Certain strokes may aggravate existing disc issues if the core is weak.
Symptoms
Herniated disc symptoms vary depending on where the disc is damaged and how much it presses on nearby nerves. Common signs include:
- Lower back pain that may worsen with movement
- Sharp, shooting leg pain caused by nerve compression (sciatica)
- Pain that increases with coughing, sneezing, or bending
- Numbness or tingling in the leg or foot
- Muscle weakness
- Difficulty standing or walking for long periods
Sometimes a lumbar disc herniation causes leg pain without back pain, making it harder to diagnose.
When to see a doctor
You should see a doctor if your symptoms don’t improve after a few days or if the pain is severe. Seek immediate care if you notice:
- Progressive weakness in your legs
- Numbness around the groin area
- Difficulty controlling bowel or bladder function
During your appointment, your doctor will ask about your symptoms, physical activity, and any past back injuries. A physical exam may include a straight-leg raise test to check for nerve irritation. Imaging tests, such as an X-ray, can rule out other causes, while an MRI is typically used to confirm a Lumbar Disc Herniation.
Non-operative treatment
Most cases of herniated discs improve with non-surgical care. Treatments may include:
Rest
Avoid activities or sports that worsen pain, especially movements involving bending or heavy lifting.
NSAIDs
Over-the-counter anti-inflammatory medications like ibuprofen or naproxen may help reduce pain and swelling.
Muscle Relaxers
These may be prescribed if muscle spasms are contributing to pain.
Physical Therapy
A physical therapist or athletic trainer will guide you through stretching and strengthening exercises to improve mobility, stabilize your spine, and reduce nerve pressure.
Steroid Injections
If symptoms remain severe, a doctor may recommend a corticosteroid injection, guided by X-ray, to reduce inflammation and relieve nerve compression.
Try these exercises to help address your condition:
Below is a PDF of the Exercise Program
Surgical Treatment
Surgery is considered only when conservative treatments fail to relieve symptoms or when nerve compression causes significant weakness. Common surgical options include:
- Microdiscectomy: Removal of the portion of the disc pressing on the nerve.
- Laminectomy: Removal of part of the vertebra to create more space for the nerves.
- Disc replacement (rare): Replacing the damaged disc with an artificial one.
Surgery often provides quick relief from leg pain, especially in cases of severe sciatica.
Recovery
Recovery varies depending on the severity of the herniation and the treatment chosen. Most people improve within a few weeks with non-surgical care. A gradual return to activity is important to avoid re-injury. Strengthening the core, maintaining a healthy weight, and practicing good posture can help prevent future disc problems.
If surgery is required, patients typically resume light activities within a few weeks and slowly return to sports based on their doctor’s guidance. Long-term rehabilitation focuses on flexibility, spinal stability, and building balanced strength.
Dr. Jay Kimmel is a board-certified orthopedic surgeon specializing in sports medicine, arthroscopic surgery, and shoulder and knee disorders. He completed his orthopedic training at New York-Presbyterian/Columbia University Medical Center and a Sports Medicine Fellowship at Temple University.
Dr. Kimmel previously served as the Director of the Connecticut Sports Medicine Institute at Saint Francis Hospital and has held faculty appointments as Clinical Assistant Professor in the Departments of Orthopedics and Family Medicine at the University of Connecticut. He has extensive experience caring for athletes as a team physician for high school and collegiate programs and continues to teach in the athletic training departments at Westfield State University and Springfield College.
Find the Support You Need — Right When You Need It
Whether you’re managing pain for the first time, need ongoing guidance, or require expert medical care, we’re here to help you every step of the way.
ORTHO DIRECT
Video visit with an orthopedic doctor for advice and a care plan.
$30
/MonthMRI DIRECT
Fast, affordable MRI with orthopedic review. No insurance required.
$499
/MonthFrequently Asked Questions
How long does it usually take to diagnose lumbar disc herniation correctly?
Most diagnoses are made within a few days to a few weeks, depending on symptom severity and whether imaging is required.
What happens if a herniated lumbar disc is left untreated or misdiagnosed?
Pain may worsen, and long-term nerve compression can lead to weakness or permanent nerve damage.
How long does non-surgical treatment for lumbar disc herniation typically last?
Most people improve within 4–12 weeks with rest, medication, and physical therapy.
When should I be concerned that my lumbar disc herniation treatment isn't working?
If symptoms don’t improve after several weeks, or if you develop new weakness, numbness, or bladder/bowel changes, you should return to your doctor immediately.