Iliotibial (IT) Band Tendonitis of the Hip Treatment
Iliotibial (IT) Band Tendonitis is an overuse injury causing pain on the outer knee or hip. It occurs when the IT band, a thick tissue running along the thigh, becomes tight or inflamed from repetitive motion. Treatments commonly include rest, stretching, strengthening, and physical therapy in runners and cyclists.
Start with our quick Symptom Assessment or connect directly with an Upswing Coach today.
Request an AppointmentReady to take the next step?
Start your symptom assessment or connect with a coach instantly.
Find Relief TodayOverview
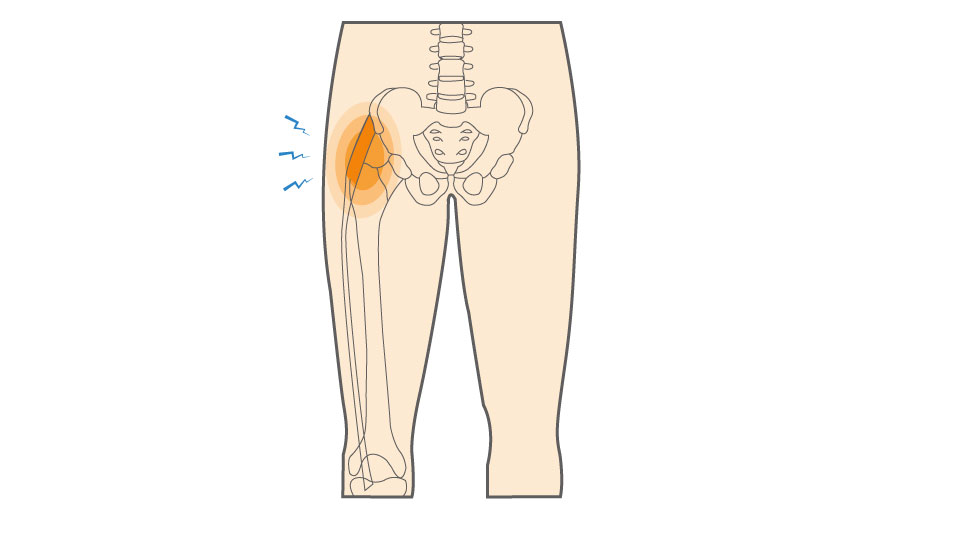
Iliotibial band (IT) tendonitis, also known as iliotibial band (IT) syndrome, is an overuse injury marked by irritation and inflammation of the iliotibial band, a thick strip of connective tissue running along the outer thigh. This band extends from the hip down to the knee, linking the gluteal and hip muscles to the upper part of the shin bone.
The IT band stabilizes the knee and supports smooth leg movement during walking, running, or cycling. When it becomes tight or inflamed, it causes pain and discomfort along the outer knee or thigh. This condition is especially common among runners, cyclists, and individuals frequently engaging in repetitive lower-body movements.
What causes Iliotibial (IT) Band Tendonitis of the Hip?
Iliotibial (IT) band tendonitis is a non-traumatic injury typically caused by repetitive stress and overuse. It commonly affects runners and athletes whose IT band becomes tight, strained, or inflamed from repeated friction over the hip bone. Over time, this irritation leads to pain and restricted mobility if not managed properly.
- How the Injury Occurs: The IT band moves back and forth over the hip and knee joints during movement. When it becomes tight, this motion creates friction and irritation against the bone, resulting in inflammation and pain. Over time, repeated strain without rest or stretching worsens the condition.
- Common Everyday Causes: IT band tendonitis can also affect people with physically demanding jobs or repetitive movement patterns, such as warehouse workers, dancers, construction workers, and even office professionals who sit for prolonged hours without proper posture or stretching.
Common Causes of IT Band Tendonitis:
- Overtraining: Excessive running or sudden increases in workout intensity can overload the IT band, leading to inflammation.
- Running on One Course: Consistently running on the same side of a sloped road causes uneven stress on the legs, tightening the outer thigh.
- Worn-Out Footwear: Old or unsupportive shoes fail to absorb shock properly, increasing strain on the hip and knee joints.
- Improper Foot Mechanics: Flat feet, overpronation, or poor gait alignment can alter leg movement, creating extra tension on the IT band.
- Insufficient Stretching: Neglecting flexibility exercises prevents proper muscle recovery and contributes to hip and thigh stiffness.
If left untreated, this overuse injury can lead to persistent pain in the outer hip and reduced mobility.
Iliotibial (IT) Band Tendonitis Is Common In:
- Long-distance or marathon running: Continuous repetitive motion and extended mileage increase the risk of IT band irritation.
- Soccer: Quick direction changes and kicking repeatedly engage the outer hip muscles.
- Tennis: Sudden lateral movements and sprints can tighten the IT band over time.
Symptoms
Iliotibial (IT) band tendonitis often develops gradually, and its symptoms can range from mild discomfort to persistent pain that interferes with daily movement. You may be experiencing IT band tendonitis if you notice one or more of the following:
- Pain or tenderness on the outer side of the hip: This discomfort often radiates along the IT band and may feel sharp or aching, especially during physical activity.
- Pain when lying on the affected hip: Pressure on the irritated area while sleeping or resting can worsen soreness and disrupt sleep.
- Increased pain when climbing or descending stairs: Movements that involve repeated bending and straightening of the hip or knee can aggravate inflammation and friction in the IT band.
The pain may sometimes extend down the outer thigh toward the knee or worsen after prolonged sitting or standing. These symptoms are hallmark signs of hip-related IT band syndrome and should not be ignored, as early treatment can prevent chronic pain and mobility issues.
When to see a doctor
If you experience persistent pain on the outer side of your hip that does not improve with rest, stretching, or basic home care, it’s important to schedule an appointment with an orthopedic specialist. This ongoing discomfort may signal inflammation or irritation of the iliotibial (IT) band that requires professional evaluation.
During your visit, the doctor will gently press on the outer hip to examine the affected area for tenderness. They may also assess your leg’s flexibility and range of motion using specific physical tests, such as Ober’s test, which helps identify tightness or tension in the IT band.
To confirm the diagnosis and rule out other possible causes of hip pain, such as arthritis, bursitis, or a stress fracture, your doctor may recommend imaging tests like:
- X-ray: To visualize bone structure and rule out joint or skeletal issues.
- MRI: To provide detailed images of soft tissues, including muscles, tendons, and ligaments, and detect inflammation or tears.
Early diagnosis ensures appropriate treatment and helps prevent the condition from becoming chronic or severely limiting mobility.
Non-operative treatment
Iliotibial (IT) band tendonitis is typically managed with conservative, non-surgical methods to reduce pain, improve flexibility, and prevent recurrence. Early intervention and consistent care are key to a full recovery.
Common Treatments Include:
- Rest: Limiting high-impact or repetitive activities allows inflammation to subside and prevents further irritation.
- IT band stretches: Regular stretching helps release tension in the IT band and surrounding muscles, improving flexibility and mobility. This is one of the most essential steps in recovery.
- Non-steroidal anti-inflammatory medications (NSAIDs): Over-the-counter options like ibuprofen can help reduce lateral knee pain and swelling associated with inflammation.
Because improper training habits or poor foot mechanics often contribute to IT band tendonitis, your doctor may also recommend preventive measures such as:
- Correcting training errors: Adjusting running form, surface selection, or workout intensity can reduce strain on the IT band.
- Choosing appropriate footwear: Wearing supportive shoes that promote proper foot alignment helps distribute pressure evenly and reduces the risk of reinjury.
These combined approaches are essential for managing hip IT band syndrome, maintaining long-term joint health, and preventing future overuse injuries.
Try these exercises to help address your condition:
Below is a PDF of the Exercise Program
Surgical Treatment
Surgery is rarely necessary for iliotibial (IT) band tendonitis, as most cases respond well to conservative, non-operative treatments. With proper rest, physical therapy, foam roll & stretching, inflammation and pain usually subside over time. In fact, most patients with outer hip or lateral thigh friction caused by IT band irritation recover fully without surgical intervention.
Recovery
You can safely return to training or sports once pain has resolved and flexibility in the affected leg has been restored. Recovery should be gradual—avoid jumping back into intense activity too quickly, as this can aggravate the injury. During rehabilitation, it’s essential to:
- Warm up properly before exercising to prepare the muscles and joints.
- Stretch thoroughly before and after physical activity to maintain flexibility and prevent tightness.
- Increase activity levels slowly to allow the IT band and surrounding muscles to adapt.
Successful recovery from hip IT band syndrome requires patience, consistent stretching, proper footwear, and mindful post-exercise care. With these steps, most individuals can resume their normal activities without recurrence of pain.
Dr. Jay Kimmel is a board-certified orthopedic surgeon specializing in sports medicine, arthroscopic surgery, and shoulder and knee disorders. He completed his orthopedic training at New York-Presbyterian/Columbia University Medical Center and a Sports Medicine Fellowship at Temple University.
Dr. Kimmel previously served as the Director of the Connecticut Sports Medicine Institute at Saint Francis Hospital and has held faculty appointments as Clinical Assistant Professor in the Departments of Orthopedics and Family Medicine at the University of Connecticut. He has extensive experience caring for athletes as a team physician for high school and collegiate programs and continues to teach in the athletic training departments at Westfield State University and Springfield College.
Find the Support You Need — Right When You Need It
Whether you’re managing pain for the first time, need ongoing guidance, or require expert medical care, we’re here to help you every step of the way.
ORTHO DIRECT
Video visit with an orthopedic doctor for advice and a care plan.
$30
/MonthMRI DIRECT
Fast, affordable MRI with orthopedic review. No insurance required.
$499
/MonthFrequently Asked Questions
Can IT band tendonitis go away on its own?
Mild cases may improve with rest and simple at-home care, such as icing and stretching. However, if symptoms persist or worsen, medical evaluation is necessary. Ignoring the pain can lead to chronic issues or compensatory injuries in other areas.
How can I prevent IT band tendonitis from coming back?
Prevention involves a combination of proper stretching, strengthening exercises (especially for the hips and glutes), wearing appropriate footwear, and avoiding training errors such as overuse or poor form. Incorporating a warm-up and cool-down into your workout routine is also key.
Is it okay to continue exercising with IT band tendonitis?
It’s best to avoid high-impact activities, especially running, while symptoms are present. Instead, opt for low-impact exercises like swimming or cycling at a low resistance. Always consult your doctor or physical therapist before resuming your training routine.
How long does it usually take to recover from a running injury like IT band syndrome?
Recovery can take anywhere from 2 to 8 weeks with non-operative treatments, depending on the severity and adherence to stretching and strengthening routines.