Hallux Rigidus Causes, Symptoms & Treatment Options
Hallux rigidus, often called “stiff big toe,” is a painful form of big toe arthritis that affects the metatarsal-phalangeal (MTP) joint. This joint is the most common place in the foot to develop arthritis. When the joint becomes stiff or loses mobility, simple activities like walking, running, or squatting can become uncomfortable and limiting. Over time, the stiffness may worsen, especially with repeated activity. Most cases can be managed with proper footwear, activity changes, and supportive treatments, but more severe cases may require surgery.
Start with our quick Symptom Assessment or connect directly with an Upswing Coach today.
Request an AppointmentReady to take the next step?
Start your symptom assessment or connect with a coach instantly.
Find Relief TodayOverview
Hallux rigidus, commonly known as “stiff big toe,” is a degenerative arthritic condition that affects the MTP joint at the base of the big toe. This joint plays an important role in balance and forward motion while walking. Because of this, arthritis in the big toe joint often leads to pain, loss of motion, and difficulty with daily activities.
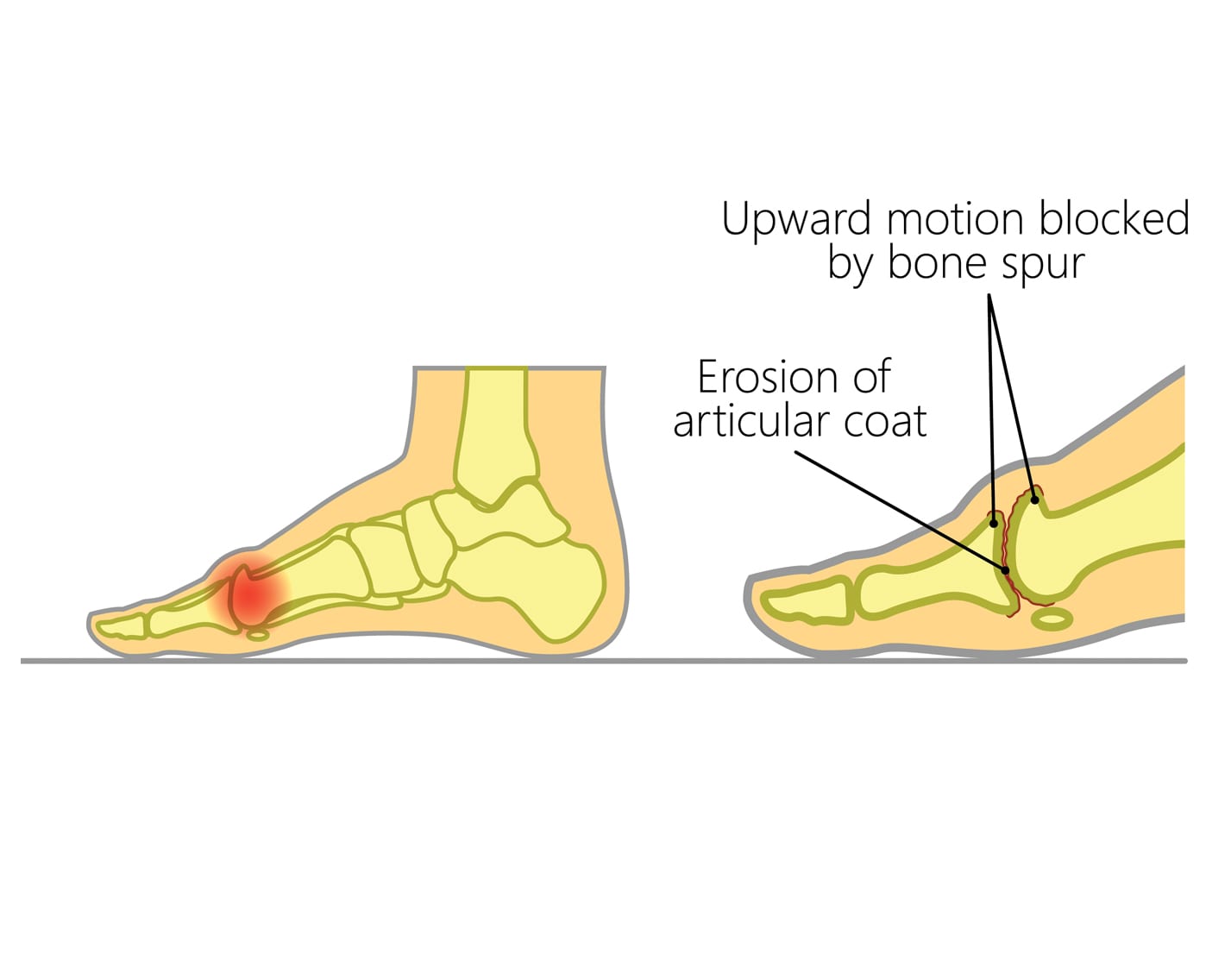
In many people, symptoms begin gradually. You may notice mild soreness after long walks or stiffness when bending the toe upward. As the condition progresses, movement becomes more restricted, and the joint can develop bone spurs on top of the toe. These bony bumps may make wearing regular shoes uncomfortable. Activities like running, squatting, or climbing stairs often increase hallux rigidus symptoms, especially as the joint becomes more arthritic over time.
What causes Hallux Rigidus?
The exact cause of hallux rigidus is not always clear, but several factors can contribute to the condition:
- Overuse and Repetitive Stress: Repeated pressure on the big toe, such as frequent squatting or pushing off during sports, can wear down the cartilage and lead to arthritis.
- Previous Injury: A past injury, such as “turf toe,” can damage the cartilage of the MTP joint. Even if symptoms improve at the time, long-term joint wear can later lead to hallux rigidus.
- How the Condition Develops: As cartilage breaks down, the joint becomes inflamed and stiff. The body sometimes forms bone spurs around the toe in an attempt to stabilize the joint, but this can actually limit motion further and increase pain.
- Common Everyday Causes: Daily habits like wearing tight shoes, standing for long hours, or walking on hard surfaces can worsen symptoms or increase the risk of developing the condition.
Sports Where Hallux Rigidus Is Common
Hallux rigidus often affects athletes who repeatedly push off the big toe or place stress on the front of the foot, including:
- Basketball: jumping and quick direction changes
- Baseball: especially catchers who squat frequently
- Softball: repetitive forward motion
- Dance: strong toe extension and balance
- Football: forceful push-off movements
- Tennis: sudden stops and pivots
Symptoms
The most common symptoms of hallux rigidus include:
Pain and Swelling
You may feel soreness at the base of the big toe, especially during walking or exercise. Swelling around the joint is common during flare-ups.
Joint Stiffness
Limited movement in the big toe, especially upward bending (dorsiflexion), is often the first noticeable sign. This stiffness can make it hard to walk normally.
Bone Spurs or Bumps
A bump may form on top of the big toe joint, which can rub against shoes and create discomfort.
Dorsiflexion Pain
Activities that require bending the toes upward, like running, climbing stairs, or pushing off during walking, may trigger sharp or aching pain.
When to see a doctor
Schedule an appointment with an orthopedic specialist if:
- You have persistent pain in the big toe.
- Bending the toe upward or downward becomes difficult.
- Walking normally is challenging.
- You notice a growing bump on top of the toe or increasing stiffness.
During your visit, your doctor will ask about your symptoms and daily activities. They will examine the toe for tenderness, swelling, and limited motion. X-rays may be ordered to check for bone spurs, joint space narrowing, or other signs of arthritis.
Non-operative treatment
In mild to moderate cases, non-surgical care can greatly reduce symptoms and slow the progression of hallux rigidus. Treatment options include:
Supportive Footwear
Switch to shoes with a cushioned, stiff rocker-bottom sole and a roomy toe box. This reduces pressure on the big toe and helps you move more comfortably. Avoid flip-flops, flexible-sole shoes, and high heels.
Orthotics
A semi-rigid or rigid Morton’s extension orthotic can help support the big toe and limit painful motion.
Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen help reduce pain and inflammation.
Steroid Injections
Your orthopedic specialist may inject corticosteroids into the joint to decrease inflammation and provide temporary relief.
Exercises
Special exercises can help maintain the range of motion, loosen tight tissues, and improve overall foot function. Your doctor or physical therapist may provide a structured program.
Try these exercises to help address your condition:
Below is a PDF of the Exercise Program
Surgical Treatment
If conservative hallux rigidus treatment fails or symptoms become severe, surgery may be recommended. The best procedure depends on how advanced the arthritis is.
Cheilectomy
Used for moderate cases. Bone spurs are removed to reduce pain and improve motion.
Osteotomy
A small wedge of bone may be removed to create more space in the joint, improving flexibility and reducing pressure.
Arthrodesis (Fusion)
For severe arthritis where cartilage is badly damaged. The bones of the joint are fused together. You will no longer be able to bend the toe, but this procedure reliably eliminates pain and restores stability.
Recovery
Your hallux rigidus surgery recovery timeline depends on the severity of your condition and the type of treatment performed.
- After a cheilectomy: weight bearing and physical therapy typically begin within two weeks.
- After an osteotomy or fusion: healing may take up to three months.
After surgery, a boot or special shoe is needed to protect the toe. Physical therapy helps restore strength and improve walking mechanics.
Dr. Jay Kimmel is a board-certified orthopedic surgeon specializing in sports medicine, arthroscopic surgery, and shoulder and knee disorders. He completed his orthopedic training at New York-Presbyterian/Columbia University Medical Center and a Sports Medicine Fellowship at Temple University.
Dr. Kimmel previously served as the Director of the Connecticut Sports Medicine Institute at Saint Francis Hospital and has held faculty appointments as Clinical Assistant Professor in the Departments of Orthopedics and Family Medicine at the University of Connecticut. He has extensive experience caring for athletes as a team physician for high school and collegiate programs and continues to teach in the athletic training departments at Westfield State University and Springfield College.
Find the Support You Need — Right When You Need It
Whether you’re managing pain for the first time, need ongoing guidance, or require expert medical care, we’re here to help you every step of the way.
ORTHO DIRECT
Video visit with an orthopedic doctor for advice and a care plan.
$30
/MonthMRI DIRECT
Fast, affordable MRI with orthopedic review. No insurance required.
$499
/MonthFrequently Asked Questions
Can I still walk or exercise with hallux rigidus?
Yes, but you may need to limit high-impact activities. Supportive shoes and modified exercises can help reduce pain.
Is surgery always needed for hallux rigidus?
No. Many people improve with conservative care such as orthotics, NSAIDs, and better footwear.
How long is recovery if I need surgery?
Recovery varies between two weeks and three months, depending on the procedure and severity of the condition.
What can I do to prevent hallux rigidus from getting worse?
Wear supportive shoes, avoid high heels, use orthotics if recommended, and stay consistent with gentle stretching and strengthening exercises.