Lumbar Degenerative Disc Disease Symptoms & Treatment
Degenerative disc disease of the lumbar spine is a condition that develops when one or more spinal discs in the lower back begin to wear down over time. These changes are often age-related and can lead to chronic lower back pain, stiffness, and reduced mobility. While disc degeneration itself is a normal part of aging, it becomes a medical condition when it starts causing pain or nerve-related symptoms.
Start with our quick Symptom Assessment or connect directly with an Upswing Coach today.
Request an AppointmentReady to take the next step?
Start your symptom assessment or connect with a coach instantly.
Find Relief TodayOverview
The lumbar spine refers to the lower portion of the spine, which consists of five vertebrae (L1–L5). These vertebrae are the primary bones in the lower back and play a crucial role in supporting body weight, enabling movement, and protecting spinal nerves.
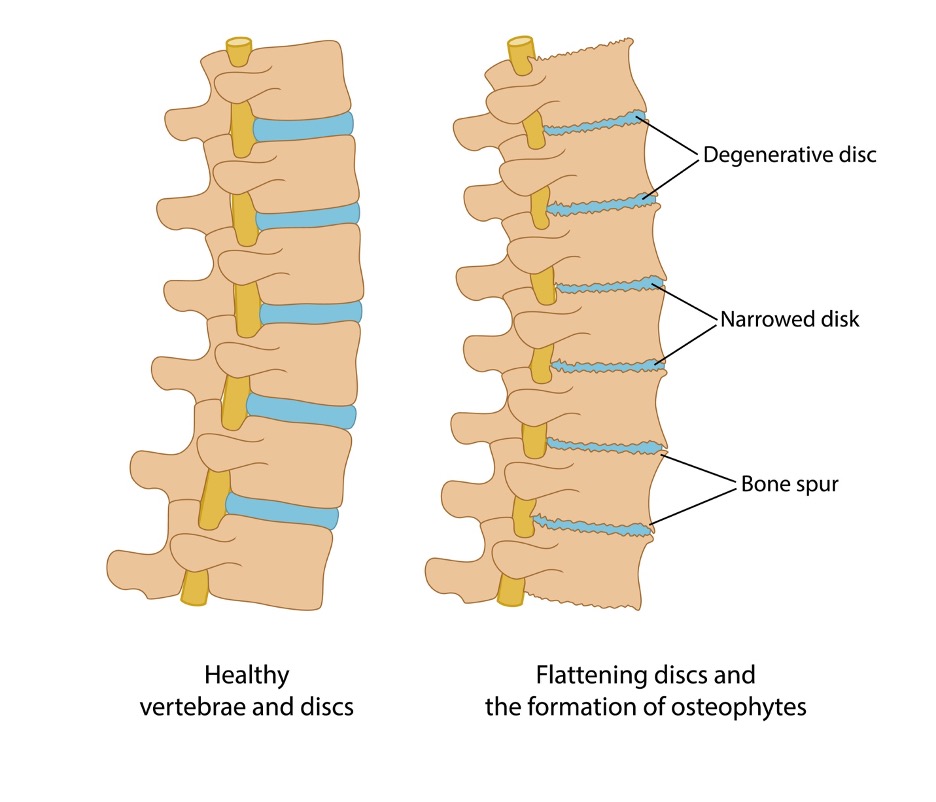
Between each lower back bone is a spinal disc that acts as a cushion. These discs absorb shock during activities such as walking, lifting, and bending. When discs lose hydration, elasticity, or height over time, they may no longer protect the vertebrae effectively, leading to pain and instability. This process is known as degenerative disc disease.
Understanding the structure of the lower back helps explain why worn or damaged discs in this area often cause pain. The lower back supports much of the body’s weight and is exposed to daily stress from activities such as standing, walking, bending, and lifting.
How Degenerative Disc Disease Develops
Degenerative disc disease happens when the spinal discs change or become damaged in different ways, such as:
Bulge
The disc protrudes outward beyond its normal boundary, which can irritate nearby nerves and cause lower back pain.
Hernia
The inner disc material pushes through the outer layer of the disc, potentially compressing spinal nerves and causing pain that may radiate into the legs.
Crack
Small tears can develop in the outer layer of the disc, leading to inflammation and pain with movement.
Thinning
Loss of disc height reduces the space between vertebrae, increasing stress on the lower back bones and joints.
Any of these disc injuries can contribute to instability and pain in the lumbar spine.
What causes Degenerative Disc Disease (Lumbar Spine)?
The lumbar spine experiences constant stress from standing, walking, lifting, twisting, and bending. As part of the natural aging process, spinal discs gradually lose water content, becoming stiffer and less flexible. This dehydration reduces their ability to absorb shock.
Over time, disc degeneration combined with arthritis of the spine (lumbar spondylosis) can lead to chronic lower back pain. Poor posture, repetitive strain, previous injuries, and genetics can also accelerate disc degeneration.
Sports Associated With Lumbar Degenerative Disc Disease
Degenerative disc disease of the lumbar spine is more common in individuals who currently play or have previously played high-impact or repetitive-stress sports, including:
- Gymnastics – repeated spinal extension and flexion
- Hockey – frequent collisions and rotational stress
- Soccer – twisting, sprinting, and impact forces
- Weightlifting – heavy axial loading on the lower back
These activities place repeated strain on the bones in the lower back and spinal discs.
Symptoms
The most common symptom of lumbar degenerative disc disease is persistent pain in the lower back and buttocks. This pain is often worse with sitting, bending, twisting, or lifting and may improve with walking or changing positions.
Additional symptoms include:
Lower back stiffness
Reduced flexibility, especially after periods of rest or inactivity.
Numbness or tingling in the legs or feet
This may occur if degenerated discs compress nearby spinal nerves.
Weakness in the legs
Nerve compression can interfere with muscle strength, affecting balance and walking.
Symptoms can range from mild to severe and may fluctuate over time.
When to see a doctor
If you experience ongoing lower back pain that interferes with daily activities, you should see an orthopedic specialist. Symptoms such as numbness, tingling, or weakness in the legs may indicate nerve involvement and require prompt evaluation.
Your doctor will review your symptoms, medical history, and perform a physical examination to assess spinal tenderness, flexibility, and range of motion.
Imaging Tests Used for Diagnosis
To confirm a diagnosis and evaluate lower back anatomy, your doctor may order:
- X-rays to assess alignment and degeneration of the lower back bones
- CT scan to provide detailed images of bone structures
- MRI to evaluate disc health and nerve compression
Non-operative treatment
Many patients find relief through conservative lumbar spine treatment options. Non-operative care focuses on reducing pain, improving mobility, and preventing further degeneration.
Common treatments include:
- Avoiding high-impact activities, such as jogging, and choosing low-impact exercises like walking
- Limiting heavy lifting and activities that strain the lower back
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to reduce pain and inflammation
- Steroid injections to relieve nerve irritation
- Physical therapy or chiropractic care to strengthen muscles that support the lumbar spine
Exercise Program
Targeted exercises help stabilize the lower back, improve flexibility, and reduce pain.
(Refer to the PDF Exercise Program below)
Surgical Treatment
If symptoms persist despite conservative lumbar spine treatment, surgery may be recommended to relieve pressure on spinal nerves and stabilize the spine.
Common Surgical Options Include:
Discectomy
Removal of the damaged disc portion to create space in the spinal canal and reduce nerve compression.
Artificial Disc Replacement
The damaged disc is replaced with an artificial disc to preserve motion between vertebrae.
Spinal Fusion
Two adjacent vertebrae are fused together using a bone graft to stabilize the spine and reduce pain caused by movement.
The choice of surgery depends on the severity of degeneration, symptoms, and overall spine health.
Recovery
Lumbar degenerative disc disease is a chronic condition that requires long-term management. While disc degeneration cannot be reversed, many people successfully control symptoms through lifestyle changes and non-operative treatment.
Recovery time after surgery varies by procedure:
- Discectomy or artificial disc replacement: approximately 2–3 months
- Spinal fusion: at least 6 months for full recovery
Post-surgical rehabilitation includes physical therapy to restore strength, mobility, and stability of the lumbar spine. Ongoing care is essential to protect your lower back and prevent future flare-ups.
Dr. Jay Kimmel is a board-certified orthopedic surgeon specializing in sports medicine, arthroscopic surgery, and shoulder and knee disorders. He completed his orthopedic training at New York-Presbyterian/Columbia University Medical Center and a Sports Medicine Fellowship at Temple University.
Dr. Kimmel previously served as the Director of the Connecticut Sports Medicine Institute at Saint Francis Hospital and has held faculty appointments as Clinical Assistant Professor in the Departments of Orthopedics and Family Medicine at the University of Connecticut. He has extensive experience caring for athletes as a team physician for high school and collegiate programs and continues to teach in the athletic training departments at Westfield State University and Springfield College.
Find the Support You Need — Right When You Need It
Whether you’re managing pain for the first time, need ongoing guidance, or require expert medical care, we’re here to help you every step of the way.
ORTHO DIRECT
Video visit with an orthopedic doctor for advice and a care plan.
$30
/MonthMRI DIRECT
Fast, affordable MRI with orthopedic review. No insurance required.
$499
/MonthFrequently Asked Questions
What are the common symptoms of lumbar degenerative disc disease?
Common symptoms include persistent lower back pain that worsens with sitting, bending, twisting, or lifting. Some individuals may experience stiffness, reduced mobility, or pain that radiates into the buttocks or legs. In more advanced cases, nerve compression can cause numbness, tingling, or weakness in the legs.
Can lumbar degenerative disc disease be managed without surgery?
Yes. Many people successfully manage lumbar degenerative disc disease with non-operative lumbar spine treatment. This may include physical therapy, activity modification, anti-inflammatory medications, steroid injections, and lifestyle changes. Conservative treatment is often effective in reducing pain and improving function without surgery.
What types of surgery are available for severe lumbar disc disease?
When conservative treatment fails, surgical options may be considered. These include discectomy to remove damaged disc material, artificial disc replacement to maintain motion between vertebrae, and spinal fusion to stabilize the spine by joining two lower back bones together. The appropriate procedure depends on the severity of the condition and patient-specific factors.
How long is the recovery after lumbar spine surgery?
Recovery time depends on the type of surgery performed. Patients who undergo a discectomy or artificial disc replacement may recover within two to three months. Recovery after spinal fusion surgery typically takes six months or longer, as the lower back bone must fully heal and fuse. Physical therapy is an important part of recovery for all procedures.